CORONARY ANGIOPLASTY & STENT INSERTION
What is atherosclerosis?
Atherosclerosis (sometimes called “hardening” or “clogging” of the arteries) is the buildup of cholesterol and fatty deposits (called plaque) on the inner walls of the arteries that restrict blood flow to the heart. Atherosclerosis can affect the arteries in the heart, legs, brain, kidneys and other organs.
Atherosclerotic heart disease (coronary artery disease) is the narrowing or blockage of the coronary (heart) arteries. Your coronary arteries are shaped like hollow tubes through which blood can flow freely. Normally, the walls of the coronary arteries are smooth and elastic. Atherosclerosis occurs when the normal lining of the arteries deteriorates, the walls of the arteries thicken and deposits of fat and plaque build-up on the coronary artery walls, blocking or limiting the flow of oxygen-rich blood to the heart muscle.
Without adequate blood, the heart becomes starved of oxygen and the vital nutrients it needs to work properly. This can cause chest pain called angina. When one or more of the coronary arteries are completely blocked, a heart attack (injury to the heart muscle) may occur.
What is a cardiac catheterization?
Coronary artery disease is the narrowing or blockage of the coronary (heart) arteries. After an interventional procedure, the coronary artery is opened, increasing blood flow to the heart.
Cardiac catheterization (also called cardiac cath or coronary angiogram) is an invasive imaging procedure that allows your doctor to evaluate your heart function. Cardiac catheterization is used to:
- Evaluate or confirm the presence of coronary artery disease, valve disease or disease of the aorta
- Evaluate heart muscle function
- Determine the need for further treatment (such as an interventional procedure or coronary artery bypass graft, or CABG, surgery)
During a cardiac catheterization, a long, narrow tube called a catheter is inserted through a plastic introducer sheath (a short, hollow tube that is inserted into a blood vessel in your arm or leg). The catheter is guided through the blood vessel to the coronary arteries with the aid of a special x-ray machine.
Contrast material is injected through the catheter and x-ray movies are created as the contrast material moves through the heart’s chambers, valves and major vessels. This part of the procedure is called a coronary angiogram (or coronary angiography). The digital photographs of the contrast material are used to identify the site of the narrowing or blockage in the coronary artery. Additional imaging procedures, called intra-vascular ultrasound (IVUS) and fractional flow reserve (FFR), may be performed along with cardiac catheterization in some cases to obtain detailed images of the walls of the blood vessels. Both of these imaging procedures are currently only available in specialized hospitals and research centers.
With IVUS, a miniature sound-probe (transducer) is positioned on the tip of a coronary catheter. The catheter is threaded through the coronary arteries and, using high-frequency sound waves, produces detailed images of the inside walls of the arteries. IVUS produces an accurate picture of the location and extent of plaque.
With FFR, a special wire is threaded through the artery and a vasodilator medication is given. This test is functionally performing a very high quality stress test for a short segment of the artery. What is an interventional procedure?
What is an interventional procedure?
An interventional procedure is a non-surgical treatment used to open narrowed coronary arteries to improve blood flow to the heart. An interventional procedure can be performed during a diagnostic cardiac catheterization when a blockage is identified, or it may be scheduled after a catheterization has confirmed the presence of coronary artery disease.
An interventional procedure starts out the same way as a cardiac catheterization. Once the catheter is in place, one of these interventional procedures is performed to open the artery: balloon angioplasty, stent placement, rotablation or cutting balloon.
Balloon angioplasty: A procedure in which a small balloon at the tip of the catheter is inserted near the blocked or narrowed area of the coronary artery. The technical name for balloon angioplasty is percutaneous transluminal coronary angioplasty (PTCA) or percutaneous coronary intervention (PCI). When the balloon is inflated, the fatty plaque or blockage is compressed against the artery walls and the diameter of the blood vessel is widened (dilated) to increase blood flow to the heart. This procedure is sometimes complicated by vessel recoil and restenosis.
Balloon angioplasty with stenting: In most cases, balloon angioplasty is performed in combination with the stenting procedure. A stent is a small, metal mesh tube that acts as a scaffold to provide support inside the coronary artery. A balloon catheter, placed over a guide wire, is used to insert the stent into the narrowed artery. Once in place, the balloon is inflated and the stent expands to the size of the artery and holds it open. The balloon is deflated and removed, and the stent stays in place permanently. During a period of several weeks, the artery heals around the stent. In this way, restenosis is somewhat diminished.
Angioplasty with stenting is most commonly recommended for patients who have a blockage in one or two coronary arteries. If there are blockages in more than two coronary arteries, coronary artery bypass graft surgery may be recommended.
Drug-eluting stents (DES): Drug-eluting stents contain a medication that is actively released at the stent implantation site. Drug-eluting stents have a thin surface of medication to reduce the risk of restenosis.
Concern was raised in 2006 regarding the safety of drug-eluting stents due to the risk of blood clots forming on the stent, causing a heart attack. The Food and Drug Administration (FDA) continues to feel that DES, when used according to approved indications, are safe and effective.
If you receive a drug-eluting stent, your doctor will prescribe certain medications for several months after your procedure to prevent the risk of clotting in the stent. It is extremely important to keep taking the medications as prescribed until your doctor tells you otherwise.
If you have concerns about drug-eluting stents, please talk with your physician.
Rotablation (Percutaneous Transluminal Rotational Atherectomy or PTRA): A special catheter, with an acorn-shaped, diamond-coated tip, is guided to the point of narrowing in the coronary artery. The tip spins around at a high speed and grinds away the plaque on the arterial walls. This process is repeated as needed to treat the blockage and improve blood flow. The microscopic particles are washed safely away in your blood stream and filtered out by your liver and spleen.
Cutting balloon: The cutting balloon catheter has a balloon tip with small blades. When the balloon is inflated, the blades are activated. The small blades score the plaque, then, the balloon compresses the fatty matter into the arterial wall. This type of balloon may be used to treat the build up of plaque within a previously placed stent (restenosis) or other types of blockages.
Preparing for the Procedure
Allergies:
Please discuss all of your allergies with your doctor, especially those listed below.
- IVP Dye/Contrast Agent Allergy, Iodine Allergy
- Latex/Rubber Products Allergy
Medications:
Discuss your medications with your physician – he may want to stop or adjust the doses several days prior to or on the day of the procedure, especially those listed below.
- Anticoagulant Medication
- Aspirin
- Diabetes Medications
Blood Work, EKG, Chest X-ray:
Ask your physician if all of the required pre-procedure tests have been completed or are scheduled before your cardiac catheterization procedure.
What to Bring
- We recommend bringing a family member with you to wait with you before the procedure.
- Please bring a robe with you to wear as you wait for the procedure.
- We recommend that you wear comfortable, easy-to-fold clothing.
- You may be admitted to the hospital after the procedure, so pack toiletries and any other items you would like to make your stay more comfortable. Your family member can retrieve these items from your car when you need them. Please leave all valuables at home or with a family member.
- A responsible adult MUST drive you home after the procedure. You will not be discharged unless there is someone available to drive you home.
Instructions after the Procedure
Going Home
A responsible adult MUST drive you home. You will not be discharged unless there is someone available to drive you home.
If you have more than a two-hour drive home, we suggest that you stay overnight in a hotel for your comfort. The Medical Concierge can help you make arrangements. Then have your family member drive you home the next morning, after you have rested.
During your drive home, stop every hour and walk for 5 to 10 minutes. If you are traveling home by plane, stand up to stretch your legs and walk in the aisle at least every hour. Please ask your doctor when you can resume driving.
After Coronary Angioplasty and Stent Insertion
Coronary Angioplasty procedure is a non-surgical treatment used to open narrowed coronary arteries to improve blood flow to the heart.
Instructions for going home after your procedure
Travel Information
You may be able to go home the same day as your procedure. Otherwise, you will spend the night in the hospital and go home the next day.
- If you live more than 2 hours away, we suggest you stay the night with a family member or friend in a local hotel. Cleveland Clinic’s Medical Concierge can help you make arrangements, if needed.
- During your trip home, stop every hour and walk for 5 to 10 minutes. If you are traveling by plane, stand up and walk in the aisle at least once every hour.
- If you have any questions about your ride home, please ask a member of your healthcare team.
Care for the Catheter Insertion Site
Interventional procedures may be performed in the femoral artery in the groin (in the area at the top of your thigh) or in the radial artery in your arm. You will have a bandage (dressing) over the catheter insertion/wound site.
- You can take this dressing off the morning after the procedure. The easiest way to remove it is by wetting the tape first, while showering.
- Place an adhesive bandage over the area. It is normal for the wound site to be black and blue for a couple of days. You may also notice that it looks pink and swollen, and there may be a small lump (about the size of a quarter) at the site.
- Wash the site at least once each day. Put soap on your hand or a washcloth and gently cleanse and rinse the area. Do not rub the area.
- Keep the area clean and dry, except when showering.
- Do not use creams, lotions or ointment on the wound site.
- Wear clothing that fits loosely over the wound site.
- Do not take a bath, soak in any kind of water or swim for one week after the procedure.
Activity Guidelines
Your doctor will tell you when you can get back to your normal routine. You will need to take it easy for the first two days after you are home. Expect to feel tired and weak the day after the procedure. Stand up slowly to avoid getting dizzy. Take walks around your house and plan to rest during the day.
If you had a transradial (wrist) procedure
- Do not move the wrist used in the procedure more than you need to for 24 to 48 hours after the procedure.
- Put soap on your hand or a washcloth and gently cleanse and rinse the area. Do not rub the area.
- Do not do anything strenuous for 24 hours. This includes most sports – jogging, golfing, play tennis, and bowling.
- Do not use a lawn mower, motorcycle, chainsaw or all-terrain vehicle for 48 hours.
- Do not take a bath or hold your affected wrist under water for 48 hours after the procedure. It is ok to take a shower the day after your procedure.
- Expect to feel mild tingling in your hand and tenderness at the insertion site for up to 3 days. If this lasts longer than 3 days or you have other non-emergency symptoms, call your doctor.
If your wrist bleeds once you are home, do not panic. Follow these steps to control the bleeding:
- Wash your hands and place 1 or 2 fingers over the puncture site. Keep pressure on the site to stop the bleeding. You may be able to feel your pulse as you do this.
- After 5 minutes, remove your fingers from the site to see if the bleeding has stopped.
- Once the bleeding has stopped, gently wipe the area clean and cover it with a bandage.
If your incision is in your groin
- Do not strain during bowel movements for 3 to 4 days after the procedure. This helps to prevent bleeding from the catheter insertion site.
- Do not lift anything that weighs more than 10 pounds or push or pull heavy objects for the first 5 to 7 days after the procedure.
- Do not do anything strenuous for 5 days after the procedure. This includes most sports – jogging, golfing, play tennis, and bowling.
- Go up and down the stairs more slowly than usual.
- Slowly start to do more during the week after the procedure, when you should be back to your normal routine.
- Ask your doctor when it is safe to resume sexual activity.
If the bleeding does not stop after 20 minutes, or if there is a large amount of bleeding or spurting, call 999 (DO NOT drive yourself to the hospital).
Medications
- Please review your medications with your doctor before you go home. Ask your doctor if you should continue taking the medications you were taking before the procedure.
- If you had a percutaneous intervention (PCI), you will need to take an antiplatelet medication. There are several types of this medication. The most common medications used are clopidogrel (Plavix), prasugrel (Effient) and ticagrelor (Brilinta). Ask your doctor if you have any questions about this medication. Before you go home, we will make sure you have enough of this medication to last 30 days. You will also get a prescription for a 90-day supply of medication. Do not stop taking this medication without talking to your cardiologist.
- If you have diabetes, your doctor may adjust your diabetes medications for one to two days after your procedure. You may need to stop taking Glucophage (metformin hydrochloride) or Glucovance for 48 hours after the procedure to reduce the risk of kidney problems. Please ask your doctor if you need to make any changes to your diabetes medications.
- Depending on the results of your procedure, your doctor may prescribe new medication. Please make sure you understand what medications you should be taking and how often to take them.
Fluid Guidelines
Be sure to drink eight to ten glasses of clear fluids (water is best) to flush the contrast material from your system.
VISUAL AIDS
Coronary Angioplasty
Demonstration of Stent Deployment
Blocked Coronary Artery causing a Heart Attack treated by Dr Ubaid
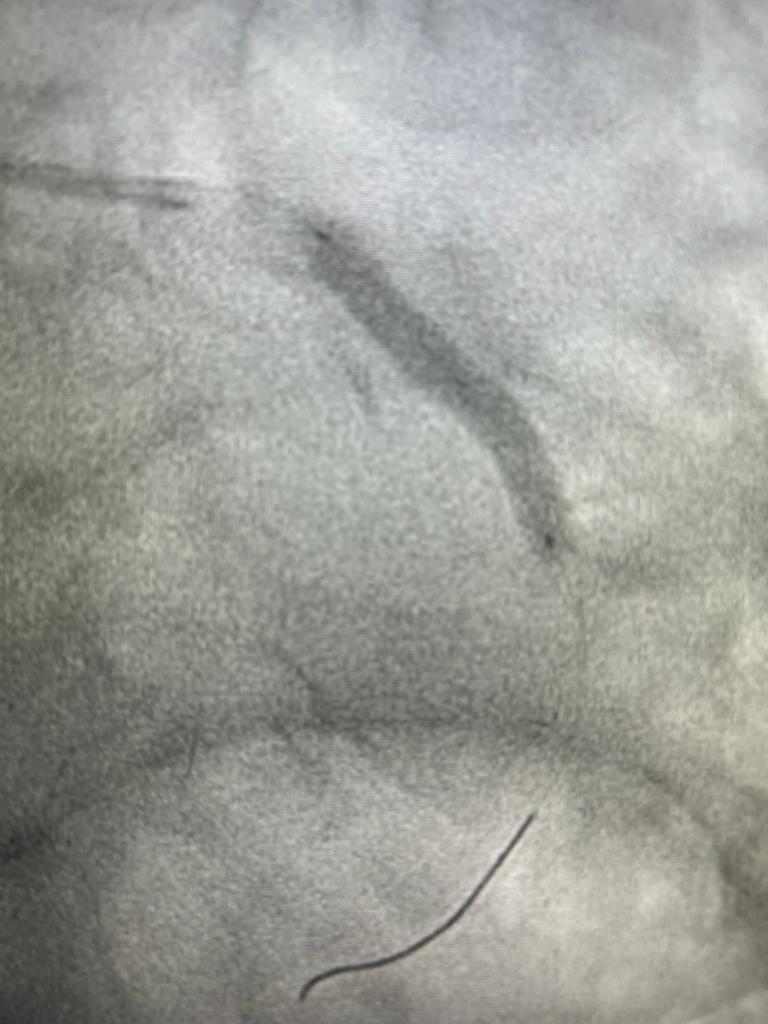
Stent Deployment during Coronary Angioplasty
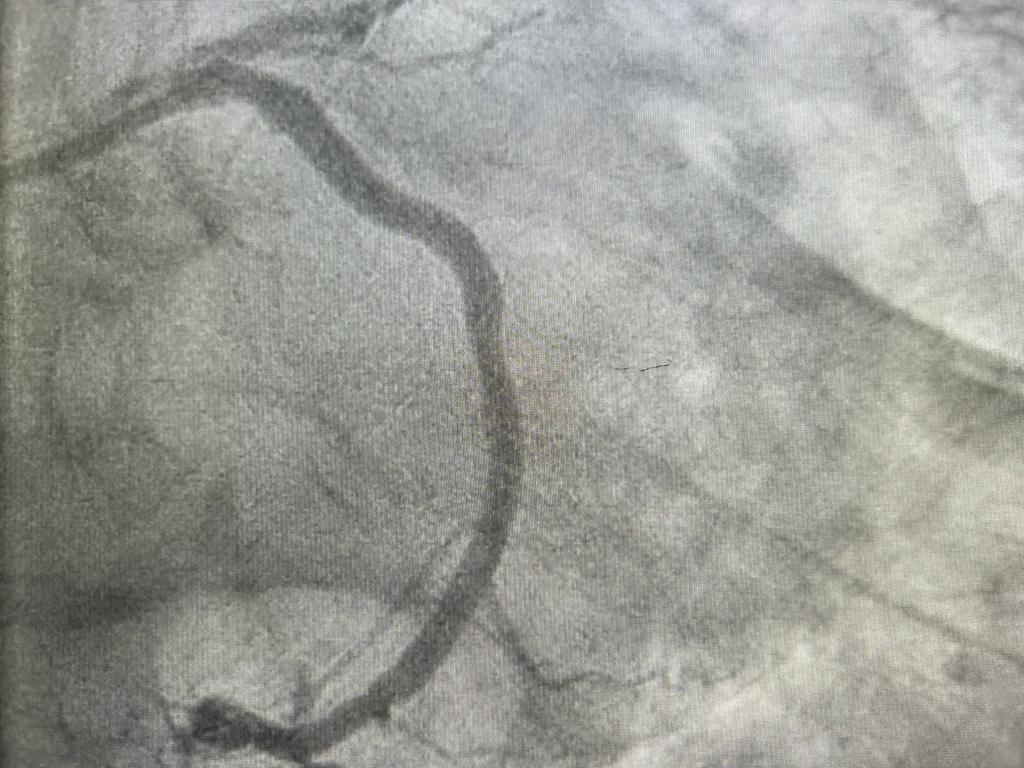
The same Coronary Artery after Stent Deployment
In life we all need role models, if I was in training to be a doctor you would certainly fit that role for me. I thank you so much for what you have done to allow me to continue with my fitness regime and wish you well in the life ahead of you.
Dr Ubaid works well with all the staff. His approach to his fellow workers is both patient and respectful. His easy going manner makes him very approachable to ask advice and he accommodates any delays graciously. I personally look forward to working with him.
His presence radiates a warmth, he instils confidence in all those around him, he sets an example for others to follow and is a role model for others to aspire to be like. He was kind, courteous, professional, understanding, caring and highly approachable and relatable as well as the medical guru we all benefit from and rely on to give us our lives back.
A great team player, all of the nursing staff are very happy to work with Salahaddin as he is polite, efficient, and has a great aura of calmness and competence and appreciates the time to be light-hearted.
What I valued as much as his erudition was his people skills, he related to everyone as an individual, his understanding, communications, interactions and personable nature were exceptional. Dr Ubaid was quite simply staggering, he is somebody that has had a significant impact on me, not just for giving me my life back and for his medical genius but for being the person that he is.
In Dr Salahaddin Ubaid I had a medical genius who also contributed significantly to aiding me overcome all of the negative worries and emotions I was feeling. The care he provided to me, his attention to detail, his personal knowledge, expertise, experience and skills was outstanding.
Your kindness and good humour were very much appreciated and certainly put me at ease throughout the procedure, which on other ocassions has been quite daunting, your relaxed approach to my problem was very calm and professional.






